

The Affordable Care Act (ACA) is a law that requires health insurance companies to provide healthcare to eligible individuals. However, the ACA does not cover everyone. For example, if you are a full-time student and you are not covered by your parents’ health plan, you are not eligible to receive the ACA premium tax credit. This is because your parents’ health plans are not ACA-compliant.
Short-term plans are not ACA compliant
Many short-term health plans do not meet the requirements of ACA-compliant health insurance. They do not offer minimum essential coverage, they may not cover pre-existing conditions, and they do not qualify for ACA subsidies. Rather than relying on a short-term plan, people with serious medical issues should consider major medical insurance, which satisfies all of the ACA’s requirements.
Despite their shortcomings, ACA-compliant plans are more affordable than you might expect. There are also some subsidies available.
In fact, in 2020, the out-of-pocket limit for a single person is $8,150. This is the same amount as the average eHealth customer paid for a short-term plan. It is important to note that these amounts are only the out-of-pocket maximums; they do not include deductibles, copays, or network restrictions.
Medicaid eligibility is determined using modified adjusted gross income (MAGI)
Most enrollees in Medicaid are eligible based on a federal income tax calculation, which is called Modified Adjusted Gross Income (MAGI). MAGI is the same measurement used for other low-income health insurance programs such as the Affordable Care Act’s Marketplace, Children’s Health Insurance Program (CHIP), and the Medicare Savings Program.
The Affordable Care Act created a uniform calculation method for most families. It also provided premium tax credits. However, there are some states that still do not have coverage. Applicants should check with their state’s Medicaid office before applying.
Before the Affordable Care Act, states had a variety of rules for determining eligibility. Many guidelines and thresholds changed each enrollment year. For example, TANF and SSI payments were no longer considered household income. In addition, inheritances, gifts, and workers’ compensation were not included.
Premium tax credit eligibility is based on estimated income
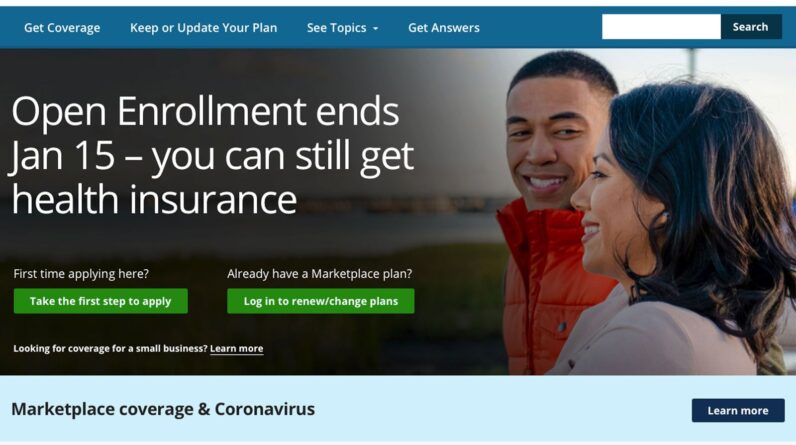
If you’re in the market for health insurance, you’ll want to consider the premium tax credit. This program is designed to help individuals and families with low income offset some of the costs of health insurance.
Eligibility is based on the household’s size and the most recent published poverty guidelines. You’ll also need to complete a Tax Form 8962 to determine your eligibility.
While there is no maximum income limit, you may have to repay a portion of the premium tax credit in your federal income tax return. Whether you’re getting a refund or owing money, keep a close eye on your taxes to make sure you’re not getting slapped with a tax bill that you can’t afford.
The premium tax credit is available to anyone who is not eligible for Medicaid or Medicare. To qualify, you must have income below 400% of the Federal Poverty Line. In addition, you’ll need to purchase a plan through the Health Insurance Marketplace.
Cost-sharing reductions are only offered through silver plans
Whether you’re shopping for a new health insurance plan or considering moving to the Marketplace, you should know about cost-sharing reductions (CSRs). These subsidies are designed to help low-income families pay their health care bills. CSRs can be used to lower deductibles and co-payments, reducing your out-of-pocket expenses.
The Affordable Care Act mandates that silver plans have CSR benefits built into them. However, you must qualify for the benefit to use it. To calculate your eligibility for CSRs, use the Yearly Income Guidelines and Thresholds Reference Guide.
Cost-sharing reductions can make a significant difference in your out-of-pocket expenses. In addition to lowering deductibles and co-payments, insurers can also reduce your out-of-pocket maximums. Some cost-sharing reduction variations are more generous than others.
Cost-sharing reductions can be extremely beneficial for low-income individuals who buy their own health insurance. While they’re a key component of the Affordable Care Act, they don’t have to be accounted for when you file your taxes.
Affordable health insurance vs employer-sponsored coverage
If you’re looking to buy affordable health insurance, it’s important to understand the differences between employer-sponsored coverage and individual plans. A job-based plan may be the most economical option for you and your family, but it’s also likely to be less comprehensive.
Despite the fact that many Americans now have access to health care, employers are finding it increasingly difficult to make their coverage affordable. As a result, workers are sacrificing wages to pay for more expensive coverage. This can create serious affordability challenges for families. Fortunately, you might be eligible for tax subsidies or a premium tax credit to help you afford coverage.
The Affordable Care Act (ACA) requires that all employers offer their employees and their dependents with health coverage. Employers can provide different types of plans to their employees, ranging from employee-only coverage to family coverage.




Comments are closed.